
Surgery is one of the first treatments a breast cancer patient receives. Research from 2014 shows that about 60% of patients with early-stage breast cancer undergo breast-conserving therapy (also known as lumpectomy)1. After breast-conserving surgery, your care team will likely recommend radiotherapy, which usually starts 4 to 6 weeks after surgery unless chemotherapy is given. In this blog, we will cover the general aspects of a lumpectomy and radiotherapy, as well as some results from recent clinical trials, and useful tips for you to manage common side effects caused by these treatments.
Breast-conserving surgery or Lumpectomy
A lumpectomy is the most frequently performed surgery. It can also be described as “breast-conserving surgery”, “partial mastectomy”, “wide local excision” or “segmentectomy”.
A lumpectomy allows cancer cells to be removed while retaining enough tissue for maintaining a normal breast shape and appearance. This procedure removes cancer, as well as the rim of healthy tissue that surrounds it. The sphere of tissue removed around the tumor is known as the “surgical margins” of cancer. You can check the status of your surgical margins in your pathology report, otherwise, ask your doctor. It is important that your surgical margins come up as “negative” or “clear” to make sure that all the cancer cells have been removed. Radiation will often follow a lumpectomy to reduce the chance of cancer returning to the site at a later date.
How do medical teams know if the margins are cancer-free? After the tumor is removed, it is color-coded with dyes for the pathologist to examine under the microscope. Sometimes, this process can be done during surgery. This way, doctors can assess if the margins of the removed tissue are free of cancer. If cancer cells are found along the margins, a wider lumpectomy or mastectomy may be needed. Additional tests will also be performed to further characterize the cancer.
What should I expect in a lumpectomy?
- A lumpectomy is usually performed as a procedure where you will return home after surgery.
- The procedure may be done under general anesthesia where medication is delivered through an intravenous line or inhaled as a gas, allowing you to sleep through the procedure. It may also be done with a local anesthetic with light intravenous sedation in which the breast area will be numb.
- The surgeon will make the incision along natural contour lines where possible to help hide the scar. The procedure usually takes from 60 to 90 minutes to complete.
Although this is the typical order of events, every patient’s lumpectomy can be different and linked to the characteristics of their tumor.
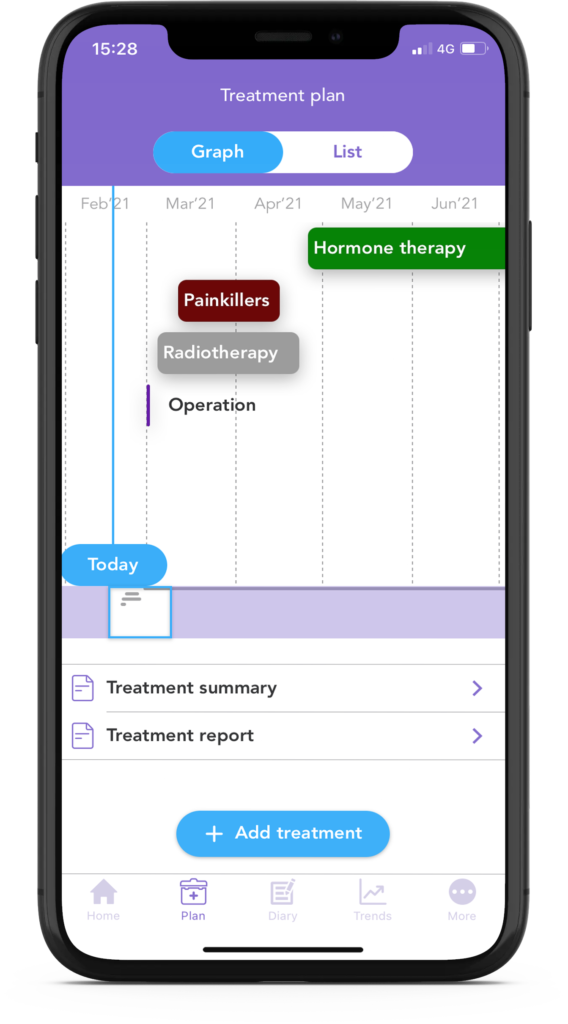
Did you know that with the OWise app, you can save all of your breast cancer treatments in one single place? … “I enjoyed using the app as it was ideal to collate all information and appointments on my treatment. Being able to collate all treatment details makes one less thing to worry about, so very important as you receive numerous letters, appointments each week” (Michelle, OWise user).
Radiotherapy
 If you have had a lumpectomy, it is likely that you will then be offered radiotherapy. This is a treatment that uses high-energy x-rays to kill cancer cells. Radiotherapy (also known as radiation therapy) is used to remove any remaining cancer cells after surgery to decrease the risk of cancer coming back. Lumpectomy followed by radiotherapy is an effective therapy to treat early breast cancer that has been trialed by a number of studies during the past two decades 2,3,4.
If you have had a lumpectomy, it is likely that you will then be offered radiotherapy. This is a treatment that uses high-energy x-rays to kill cancer cells. Radiotherapy (also known as radiation therapy) is used to remove any remaining cancer cells after surgery to decrease the risk of cancer coming back. Lumpectomy followed by radiotherapy is an effective therapy to treat early breast cancer that has been trialed by a number of studies during the past two decades 2,3,4.
The current guidelines offer whole-breast radiotherapy to anyone who has had invasive breast cancer and has been treated with a lumpectomy5. This means that high-energy rays will target the remaining cancer cells in your chest (breast) and lymph nodes.
The standard radiotherapy treatment usually lasts 5 to 8 weeks and consists of 25-28 fractions (sessions). It is usually administered 5 days a week with a break of 2 days (during weekends) between each cycle. Overall, a dose of 50 Gy is delivered by the end of the treatment (Gy means Gray, it is the unit used to measure radiation energy)11.
What is a fraction of radiotherapy? Each radiotherapy treatment is known as a fraction in which small doses of radiation are delivered. This allows healthy cells to recover after radiation. Healthy cells have a greater ability to repair DNA damage than cancer cells. As such, splitting the total radiation dose in fractions gives time to healthy cells to repair this damage. Therefore, you will receive a series of treatment sessions or fractions that will make up your radiotherapy treatment/course.
If your breast cancer is considered high risk, your doctor may recommend a radiotherapy boost of another 10-16 Gy at 1.8-2 Gy per fraction to the area where the cancer was, also known as the tumor bed5. You might be considered high-risk if you are less than 50 years old or if you have high-risk pathological features such as a Grade 3 cancer. To learn more about grading head over to our Pathology report blog.
Did you know that a recent study has shown that an injection with a simple antiseptic solution like hydrogen peroxide can make cancer cells more sensitive to radiotherapy? If you want to know more, read here6.
Partial breast radiotherapy
Partial breast radiotherapy (also known as “accelerated partial breast radiation (APBI)”) will be offered if the risk of your cancer coming back is low. A typical APBI schedule consists of a dose of 34 Gy delivered in 10 fractions twice per day by brachytherapy.
Brachytherapy is a type of radiotherapy in which a radiation source is placed inside the body area to be treated. It typically involves inserting radioactive implants into the space in the breast where the tissue has been removed. The implants are usually in place for one to five days. The aim of the procedure is to minimize the chance of cancer recurring.
People with low-risk cancer include women over 50 with tumors smaller than 2 cm, hormone receptor-positive (ER-positive), negative margins and no familiar history of cancer. This treatment can also be offered if hormone therapy (Tamoxifen or Aromatase Inhibitors) will be included in your treatment plan for a minimum of 5 years.
Some women who have had a lumpectomy may not need radiotherapy at all. This might be the case for people with a very low risk of recurrence (women over 65 with a tumor that is smaller than 2 cm, hormone receptor-positive (ER-positive), HER2-negative, grade 1-2 and with no cancer cells in their lymph nodes) and are willing to take hormone therapy for a minimum of 5 years 7.
New radiation therapy strategies
New radiation treatment strategies have been developed in recent years. The 10-year results of the FAST trial, demonstrated that a lower dose of radiotherapy (28.5-30 Gy) delivered in fewer but larger doses (6 Gy once a week) is as safe as a larger total dose of 50 Gy in daily small doses (2 Gy)7. This new strategy can be particularly beneficial for patients at low risk who cannot tolerate daily radiation over long periods of time because of frailty or other chronic conditions.
What about intraoperative radiotherapy (IORT)? IORT consists of radiation therapy given during breast-conserving surgery, right after the cancer has been removed. While the underlying breast tissue is still exposed, a single, high dose of radiation is given directly to the area where the tumor was. Recent clinical trials have demonstrated that it can be an effective alternative to external beam radiotherapy8.
There are other types of APBI like 3D-conformal radiotherapy (3D-CRT) or intensity-modulated radiotherapy (IMRT). To read more about these techniques, visit the American Cancer Society website. Also, it may be useful to speak with your doctor about the advantages and disadvantages of this treatment.
What should I expect during radiotherapy?
- Before you receive radiotherapy you will undergo the treatment planning process. This consists of a CT scan to evaluate the exact area and the most effective dose of radiation.
- During radiotherapy, you will rest on a breast board. This will be set up to your individual measurements each session to ensure your body is placed in the same position for each treatment.
- A radiotherapy appointment will last between 12 and 15 minutes. The majority of the time will be spent setting up the procedure. The treatment itself lasts about 3 or 4 minutes.
- Radiotherapy can react with metal, so they will ask you to remove any jewelry or metal-containing objects.
- During radiotherapy, you will need to lie still, though you can still breathe normally.
- The breath-hold technique can help protect the heart from being affected by radiotherapy given to the left side. For this, you will need to take a deep breath in and hold it for a short time (your radiographer will inform you when to breathe in and out).
Lymphoedema and cording due to surgery can cause discomfort in the arm and can limit mobility. Radiotherapy will be delayed until you have a full range of movement in your arm. This is because your arm needs to be above your head so that the whole breast or chest area can be treated
Radiation side effects
Due to how radiotherapy is administered, as it travels through normal healthy cells to reach the tumor, you may experience a number of side effects. The most common side effects are:
- Skin reactions – including reddening and tenderness, similar to a sunburn, becoming pinker or darker over time, peeling or blistering. This usually begins 10-14 days after starting treatment.
“After a couple of weeks, your skin will usually start to go red, like sunburn, over the area where the radiation beam passes through it. As the waves go in straight lines, your radiotherapy redness will have straight edges – and this, coupled with the fact that it’s concentrated on your breast, gives it a bizarre appearance, as if you’d been sunbathing in a very odd, and rather inappropriate, swimming costume.” (Dr Kathleen Thompson10)
 Tiredness and fatigue during treatment and a couple of weeks after treatment. This tiredness can go on for many months after treatment, but it varies from person to person.
Tiredness and fatigue during treatment and a couple of weeks after treatment. This tiredness can go on for many months after treatment, but it varies from person to person.
- To tackle this fatigue, it is good to keep hydrated, have a varied diet with plenty of fruits and vegetables, and do some light exercise such as going for short walks. You may find it useful to track your fatigue levels and physical effort with the OWise app.
- Swelling and pain of the breast or chest area.
- It is recommended to take painkillers if you need to. You may also want to wear a soft supportive bra or nothing at all.
- Change in breast size, touch (the breast may become firmer) and color (darker or lighter).
- There can be some tightening of the muscles over the chest, which means that the overall range of movement at the shoulder can be a little more restricted.
- The exercises that you are given to do after surgery are very important to avoid any movement restriction.
- A few women might experience shortness of breath or a dry cough following the radiotherapy.
Radiotherapy can be an emotionally difficult time for you as it comes at the end of months of treatments, and you are often going through the side effects of those as well. It can be a time when you look back on all that’s happened and think about what’s going to come next. Ask your care team for support to talk about your thoughts and feelings, to work through your worries and concerns.
We hope that you now better understand lumpectomy and radiotherapy treatment and that you can feel confident in discussions with your care team.
If you found this article useful and would like to access more personalised information, download OWise today.
References
- Agarwal SPappas LNeumayer LKokeny KAgarwal J. Effect of Breast Conservation Therapy vs Mastectomy on Disease-Specific Survival for Early-Stage Breast Cancer. JAMA Surg. 2014;149(3):267–274. doi:10.1001/jamasurg.2013.3049
- Clarke, M., Collins, R., Darby, S., Davies, C., Elphinstone, P., Evans, V., Godwin, J., Grat, R., Hicks, C., James, S., MacKinnon, E., McGale, P., McHugh, T., Peto, R., Taylor, C., Wang, Y. 2005.Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 366(9503), pp: 2087–2106.
- Veronesi, U., Cascinelli, N., Mariani, L., Greco, M., Sacozzi, R., Luini, A., Aguilar, M., Marubini, E. 2002. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 347(16), pp: 1227–1232.
- Fisher, B., Anderson, S., Bryant, J., Margolese, R., Deutsch, M., Fisher, E., Jeong, J., Wolmark, N. 2002.Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 347(16), pp: 1233–1241.
- Cancer.org. 2021. Radiation for breast cancer. [online] Available at: https://www.cancer.org/cancer/breast-cancer/treatment/radiation-for-breast-cancer.html
- Icr.ac.uk. 2021. Common antiseptic could be cheap and easy way to improve cancer radiotherapy around the world. [online] Available at: https://www.icr.ac.uk/news-archive/common-antiseptic-could-be-cheap-and-easy-way-to-improve-cancer-radiotherapy-around-the-world [Accessed February 2021].
- Icr.ac.uk. 2021. Long-term safety of radiotherapy in fewer doses for patients with early breast cancer demonstrated in 10-year study. [online] Available at: https://www.icr.ac.uk/news-archive/long-term-safety-of-radiotherapy-in-fewer-doses-for-patients-with-early-breast-cancer-demonstrated-in-10-year-study [Accessed February 2021].
- Vaidya, J., Baum, M., Pigorsch, S., Douek, M., Flyger, H., Brew-Graves, C., Potyka, I., Brown, D., Laws, S., Corica, T., Vinante, L., Pazos, M., Gruber, G., Dedes, K., Blohmer, J., Hoefer, R., Petralia, G., Tobia, J. 2020. Long term survival and local control outcomes from single-dose targeted intraoperative radiotherapy during lumpectomy (TARGIT-IORT) for early breast cancer: TARGIT-A randomised clinical trial. BMJ.370.
- youtube. com. 2018. Having radiotherapy for breast cancer. [online] Available at: https://www.youtube.com/watch?v=4SSTa9rMjrc
- Thomson, K. 2015. From Both Ends of the Stethoscope: Getting through breast cancer—by a doctor who knows. Faito Books.
- American Cancer Society. 2023. Getting External Beam Radiation Therapy. American Cancer Society. Available at: https://www.cancer.org/cancer/managing-cancer/treatment-types/radiation/external-beam-radiation-therapy.html#:~:text=The%20total%20dose%20of%20external,for%20normal%20cells%20to%20recover.
