What is BRCA?
BRCA stands for breast cancer susceptibility gene. There are two of these genes, BRCA1 and BRCA2, the former first discovered by Mary-Claire King in the 1980’s. Their function is to help repair damaged DNA, preventing the development of tumours. There are certain variants of these genes that can result in a loss of their function whereby the mechanism to repair DNA is compromised. This may mean that any damage to the DNA is not adequately repaired and as a result, cells are more likely to develop additional genetic alterations that can lead to cancer.
Inheritance of BRCA variant genes
 BRCA genes are hereditary, meaning you receive a copy of each gene from both parents. If someone has inherited a faulty version of the BRCA gene from one or both parents, they have an increased risk of developing breast cancer. Assembling a family history of cancer is crucial in assessing a person’s potential risk. Both first-degree (parents, siblings, children) and second-degree (aunts, uncles, cousins) relatives’ histories are required for a comprehensive evaluation. If cancer runs in your family, genetic counselling can help you to assess whether a genetic test is right for you, and help you determine whether your insurance policy covers it. This type of testing will indicate whether the person has inherited one or more cancer risk genes. Some genetic testing companies offer tests to people who are uninsured and meet medical criteria.
BRCA genes are hereditary, meaning you receive a copy of each gene from both parents. If someone has inherited a faulty version of the BRCA gene from one or both parents, they have an increased risk of developing breast cancer. Assembling a family history of cancer is crucial in assessing a person’s potential risk. Both first-degree (parents, siblings, children) and second-degree (aunts, uncles, cousins) relatives’ histories are required for a comprehensive evaluation. If cancer runs in your family, genetic counselling can help you to assess whether a genetic test is right for you, and help you determine whether your insurance policy covers it. This type of testing will indicate whether the person has inherited one or more cancer risk genes. Some genetic testing companies offer tests to people who are uninsured and meet medical criteria.
The choice of taking a genetic test is solely up to the individual. Knowledge of risk can allow for early management, including regular breast examinations, alternative screening types such as ultrasound and MRI and adopting risk reduction strategies.
Impact of prior knowledge of faulty BRCA genes
Not only does detection prior to diagnosis increase the chance of earlier detection, an Israeli study1 found that women carrying faulty BRCA1/2 genes who develop breast cancer appear to fare better if their genetic risk was detected prior to their cancer diagnosis, even if they do not undergo preventative procedures such as risk-reduction surgery.
Although the group of women with prior knowledge and those without were roughly the same age when diagnosed with cancer, those with prior knowledge of their BRCA gene status were diagnosed with less invasive forms of breast cancer compared to those unaware. They also had a higher overall survival advantage, despite similar breast cancer grades, hormone receptors status and subtypes in both groups. These effects are likely due to the increased awareness of breast cancer and therefore the ability to catch it at an earlier stage.
BRCA variant genes in the risk of cancer
In the general population, 1 in 8 women develops breast cancer during their lifetime. With a faulty BRCA gene, this risk increases. For someone with a BRCA mutation, there is a 70% chance (or 70 out of 100 people) to develop breast cancer by the age of 802. Those associated tend to develop in younger women and be present in both breasts. Of all breast cancer cases, 5-10% are associated with faulty variants of the BRCA genes. However, the profiles of the development of cancer caused by BRCA1 and BRCA2 differ as they also may cause ovarian cancer. Whilst commonly only 1 in 100 women will get ovarian cancer during their lifetime, a BRCA1 variant gene increases the incidence to 44 women. Faulty BRCA2 genes have less association with ovarian cancer, with 17 out of 100 women likely to develop it. Defective BRCA2 genes don’t just affect women. Men with a faulty BRCA2 gene are 80 times more likely to develop breast cancer, as well as 7 times more likely to develop prostate cancer.
Targeted treatments for BRCA
PARP inhibitors are an emerging treatment for BRCA positive individuals. Normally the PARP proteins help repair damaged DNA inside cells. By stopping these proteins working, on top of the decreased DNA repair from the faulty BRCA gene, the damage to the DNA often leads to the death of tumour cells.
The most common PARP inhibitor, olaparib (brand name Lynparza®) is approved by the FDA for women for people with HER2-negative, secondary breast cancer and an altered BRCA gene3 as well as people with newly diagnosed, advanced BRCA-mutated ovarian cancer.
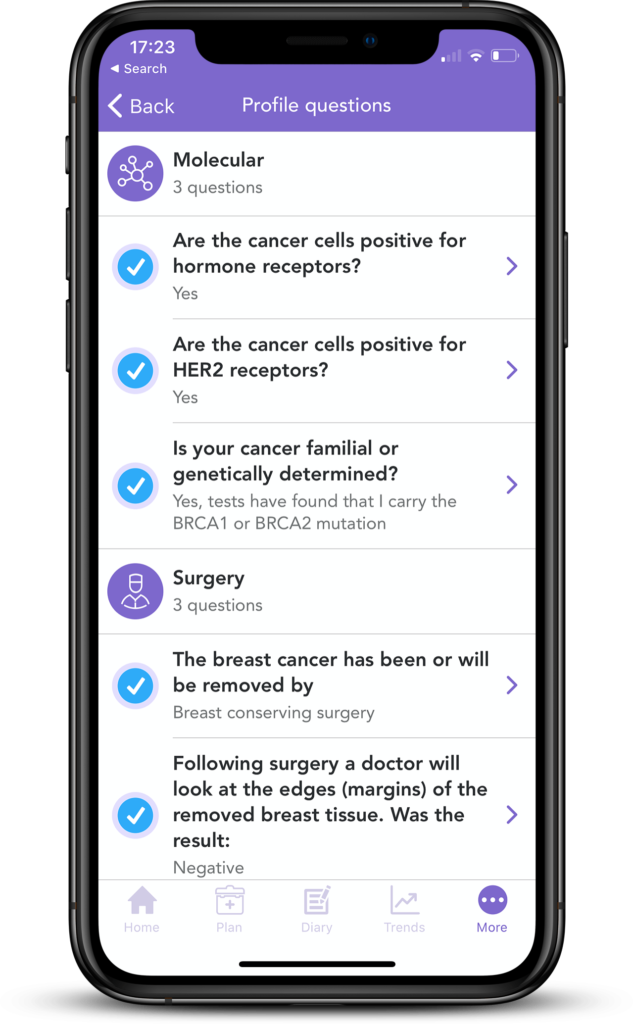
If you have been tested positive for BRCA1 or BRCA2 gene variants, you can add this into your OWise profile. Your personalised treatment report will then give you a thorough description of how this may impact screening, treatment and suggestions to manage the risk of developing cancer.
Did you find this interesting? Let us know below!
Useful links/Read more
National Breast Cancer – https://www.nationalbreastcancer.org/what-is-brca
Cancer.gov – https://www.cancer.gov/about-cancer/causes-prevention/genetics/brca-fact-sheet
Breast Cancer Org – https://www.breastcancer.org/symptoms/testing/genetic/facility_cost
Breast Cancer Now – https://breastcancernow.org/information-support/facing-breast-cancer/going-through-breast-cancer-treatment/parp-inhibitors-in-breast-cancer-treatment
References
- Hadar T, Mor P, Amit G, Lieberman S, Gekhtman D, Rabinovitch R et al. (2020) Presymptomatic Awareness of Germline Pathogenic BRCA Variants and Associated Outcomes in Women With Breast Cancer. JAMA Oncology.
- Barnes D, Phillips K, Mooij T, Roos-Blom M et al. (2017). Risks of Breast, Ovarian, and Contralateral Breast Cancer for BRCA1 and BRCA2 Mutation Carriers. JAMA. 317(23):2402-2416
-
Center for Drug Evaluation and Research. “FDA Approves Olaparib for Germline BRCA-Mutated Metastatic Breast Canc.” U.S. Food and Drug Administration, FDA, www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-olaparib-germline-brca-mutated-metastatic-breast-cancer.
