
Urogenital problems refer to issues within the urinary and genital areas, including the vulva, vagina, and lower urinary tract. Up to 50–75% of people with breast cancer experience one or more symptoms related to the genital and urinary areas1,2. These side effects are part of an array of menopausal symptoms brought on by certain breast cancer treatments, especially hormone treatments such as tamoxifen and aromatase inhibitors. This is because these treatments systematically reduce the amount of oestrogen available. This reduction in oestrogen is the main cause for urogenital side effects.
Oestrogen is a hormone that carries out important functions throughout the entire body but the effects of its reduction are more severe in urogenital areas such as the vaginal, urethra, bladder and pelvic floor muscle tissue, as they contain high concentrations of oestrogen receptors3.
In this blog we will look at the effects that breast cancer therapies can have on the urogenital area and discuss some useful tips to help you manage these side effects.
What is Genitourinary Syndrome of Menopause?
The term genitourinary syndrome of menopause (GSM) is used to include urinary, genital (vulvovaginal discomfort), and sexual dysfunction symptoms associated with menopause.
GSM symptoms can include4:
- vaginal discomfort, dryness and irritation
- painful sex (a.k.a dyspareunia)
- Irritation of urinary tract
- Discomfort/pain/burning during urination
- Recurrent and chronic UTI
- Incontinence
Vulvovaginal atrophy and breast cancer treatment
Vulvovaginal atrophy (VVA) is frequent in postmenopausal women as it is strongly associated with low oestrogen levels5. VVA includes symptoms such as vaginal dryness, burning, discharge, itchiness, irritation and bleeding 4.
These side effects are also common in oestrogen receptor positive (ER+) breast cancers. In this subtype of breast cancer, oestrogen can stimulate cancer cells to grow, and typical hormone therapies (such as tamoxifen and aromatase inhibitors) aim to prevent oestrogen reaching these cancer cells. To learn more about how hormone therapies work, check out our previous blog.
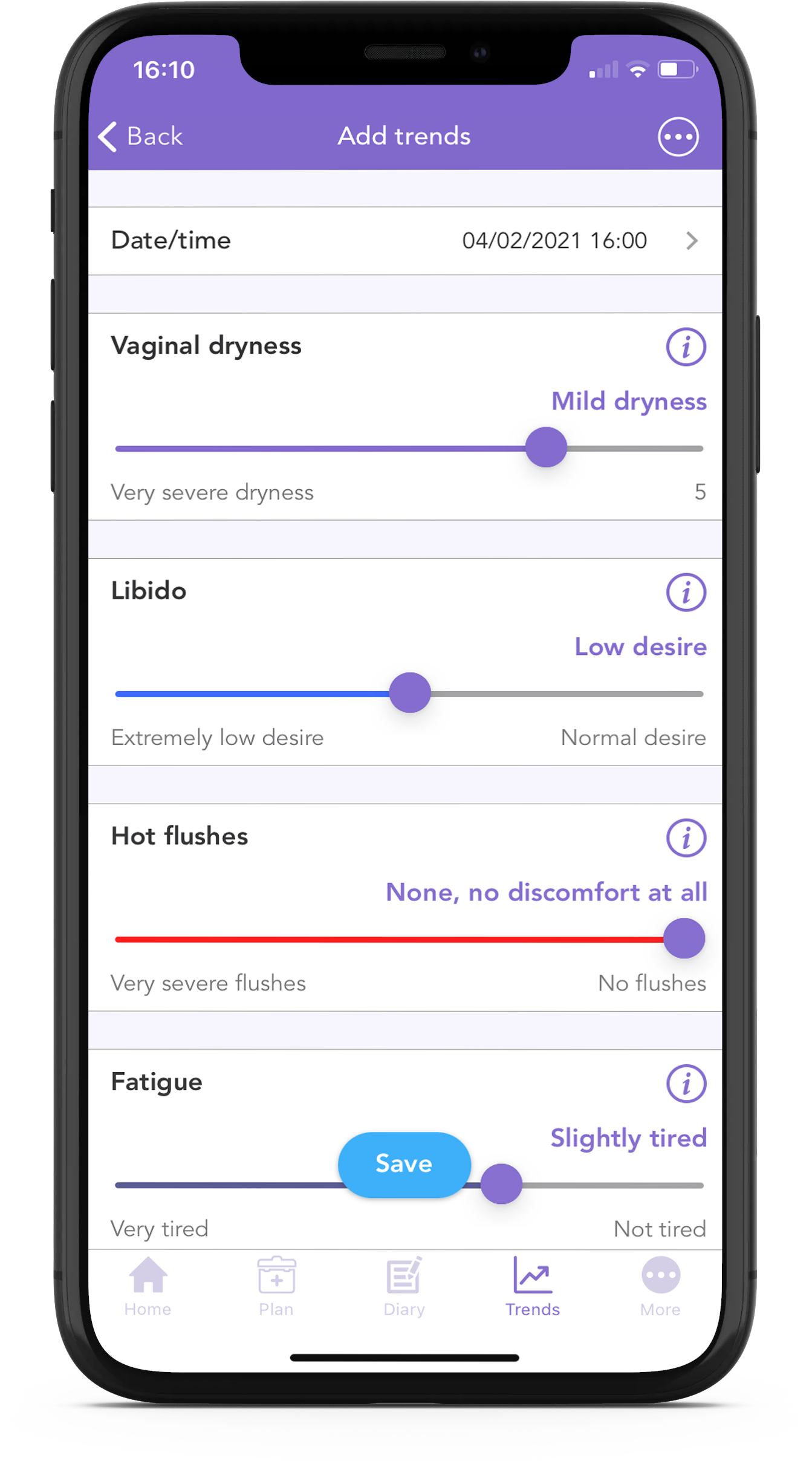
VVA symptoms are often underreported6 and can have an impact on sexual function and quality of life. It is important to recognise them and inform your clinical team. With the OWise breast cancer app you can track many side effects including your vaginal dryness!
Clinical studies have demonstrated a link between hormone therapies and VVA. For instance, a study with ER+ breast cancer patients showed that 57.6% of those on aromatase inhibitors and 32.4% on tamoxifen had at least one vaginal atrophy symptom rated as moderate to severe5. Another study demonstrated that those on anastrozole experienced more vaginal dryness than people taking tamoxifen7.
Chemotherapy can also induce the reduction of ovarian function leading to reduced oestrogen production8. Another breast cancer study investigating patients on tamoxifen and chemotherapy showed that those that remained postmenopausal after a high dose of chemotherapy still experienced vaginal dryness post chemotherapy9.
Please note that the removal of ovaries may be recommended to premenopausal women with high risk of familial breast cancer10. The removal of ovaries will lead to a reduction in oestrogen production which can increase the risk of VVA. Learn more about increased familial risk and the BRCA genes in our previous blog.
As previously mentioned, the systematic reduction of oestrogen is the main cause of VVA side effects including:10, 11
- Vaginal tissue thinning12 – less and thinner tissue layers
- Increase of vaginal pH that can trigger bacteria overgrowth such as thrush
- Decreased blood flow
- Reduced moisture secretion of the cervical glands
- Loss of elasticity
These can lead to symptoms including a dry, sore, burning or itchy vagina.
Urinary problems and breast cancer treatment
Urinary problems are common amongst the breast cancer population (both in treatment and recovery), with 12% of people reporting pain when urinating to 58% reporting bladder control issues13.
Oestrogen contributes to the elasticity and health of the urethra and pelvic floor muscles. The pelvic floor consists of muscles surrounding the lower part of the bladder and urethra. Lower levels of oestrogen can cause muscle weakening and reduced elasticity which can lead to incontinence issues14. Less healthy tissue also increases the risk of infection and feelings of irritation, even without infection. Furthermore, anticancer treatments that compromise the immune system can increase the risk of infection.
Chemotherapy increases the risk of urological issues as the bladder and urinary tract contain fast dividing cells, consequently they too are targeted by chemotherapeutic drugs. Chemotherapeutic drugs, such as ifosfamide (Ifex ®),15, 16 are also broken down into substances which can irritate the urinary system when passing urine. These processes can lead to discomfort and higher risk of infection.
Signs of urinary infection/cystitis
- urgency and frequency (a frequent and urgent need to pee)
- pain or burning when peeing
- pain in the stomach, back or sides
- blood in urine
- fever, chills and feeling ill
Reducing the risk of urinary infection
- drink lots of water. Especially before, during and after chemotherapy to dilute irritants
- urinate before and after sex
- reduce irritant intake eg. spicy/acidic foods, caffeine, carbonated drinks etc
- be aware of constipation (possible chemotherapy side effect) which can add pressure on the bladder
- reduce vaginal dryness (see below and here)
What can I do?
If you are feeling discomfort, don’t hesitate to discuss this with your oncologist, urologist or gynaecologist. It is important to notify doctors of any symptoms, as these could indicate an underlying infection which needs to be treated. There are lots of management options available and together an appropriate treatment plan can be created. The next section will explore some available management options for both GSM and urinary side effects.
If you have questions for your care team, you can note them down using the OWise Breast Cancer app and record the consultation (with permission) to refer back to later on. This way, you can make sure that you have remembered to ask all of the questions that you have and a record of the answers!
For vulvovaginal symptoms:
Topical moisturisers applied regularly introduce moisture to the area providing relief and improvements 19. A small study reported significant improvements with vitamin E and D vaginal suppositories 20.
Don’t be discouraged from engaging in sexual activity. In fact, it can help as it stimulates blood flow to the area! 21, 22 Just remember to use plenty of natural lube and no mixing oil-based with silicone. Read more about Sex, Intimacy and Breast Cancer Treatment.
“It’s really important to be aware of the ingredients of your lubricant as not all sexual lubricants and vaginal moisturisers are the same. Many products, including some available on prescription, contain irritating ingredients including glycerin, glycols and parabens, in addition to dyes, perfumes, flavouring, cooling and warming ingredients. Glycerin is a common lubricant ingredient but it can cause thrush, often prevalent post cancer treatment.” – Sam Evans, founder of Jo Divine in her Q&A with tickingoffbreastcancer
You can find more information on menopausal symptoms, vaginal dryness and irritation and their implication on sex on the Jo Divine website.
However, moisturisers and lubricants do not address the root of GSM problems: a lack of oestrogen. They only aim to soothe discomfort caused by side effects. Consequently, side effects and their discomfort may continue.
Hormonal treatments such as creams and Ospemifene oral medication 23, 24 target the root of GSM issues, a lack of oestrogen, by reintroducing oestrogen to the body. These may not be suitable for oestrogen receptor positive (ER+) breast cancers, and as such you should discuss this with your doctor 25. Localised topical oestrogen therapy, such as vaginal creams, can introduce lower doses of vaginal oestrogens. This has been shown to help ease symptoms, without affecting the level of oestrogen in the blood that could stimulate breast cancer cells 26. However, more research is needed to confirm this and you should discuss this with your care team before use 25.
Laser vaginal therapies show promising results27. However, appropriate trials with breast cancer populations need to be conducted to assess suitability. These therapies carefully heat up tissue in the vagina to activate repair processes which increase collagen and elastic fibres reducing VVA symptoms 28.
For urinary problems:
If you are experiencing pain, a urine test to check for infection is recommended.
Incontinence can be addressed with various non-invasive methods. For example, Kegel exercises are a great easy way to strengthen your pelvic floor, increasing control in the area. Studies report home Kegel exercises significantly improve a range of urinary incontinence problems29, 30.
Self-monitoring and life-style changes can also be implemented. These include bladder training such as urination scheduling and delay31. Urination scheduling involves scheduling bathroom breaks at set intervals and gradually increasing the interval. Bladder delay involves holding the urge to pee, increasing how long you resist going to the bathroom each time.
To help stick to the schedule and urination delay you can distract yourself with mindfulness techniques such as breathing exercises or counting backwards from 100. You can also start practicing delay in the bathtub to avoid any accidents.
To learn more about self-monitoring and life-style changes for urinary problems read on here.
Other lifestyle changes such as reduction in smoking can also have positive effects on vulvovaginal and urinary symptoms as cigarette smoking is associated with a faster occurrence of VVA 17 and a 3x higher risk of urinary urgency and frequency18.
Addressing, treating and improving these symptoms is not only for your quality of life but also for your safety and health. Do not hesitate to address these issues with your doctors.
Although both pre and post-menopausal women report GSM symptoms, oncologists do not commonly inform patients about these possible side effects. If your doctor does not speak about these issues feel free to bring them up. They are common, you are not alone and together they can be addressed and improved.
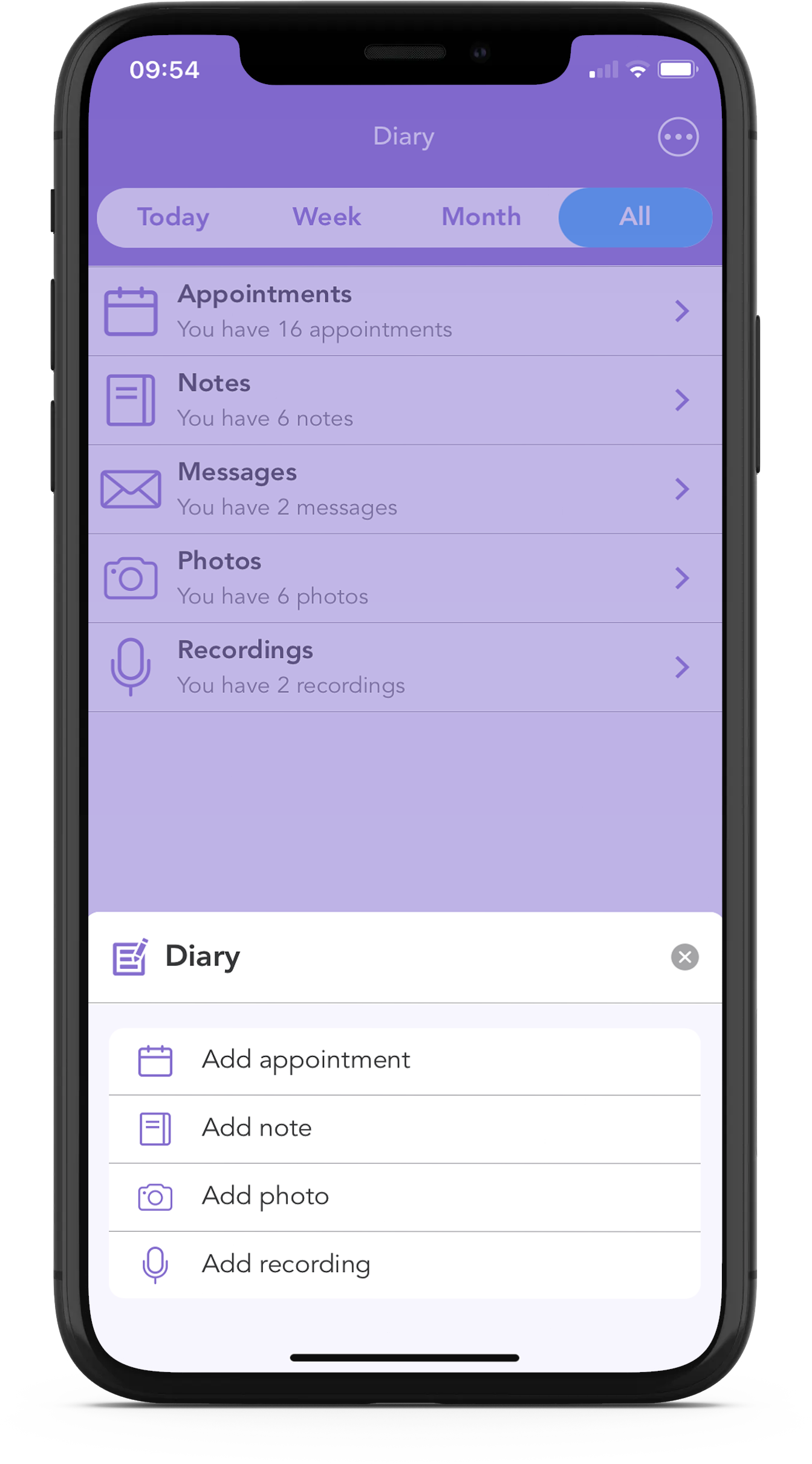
At OWise, one of our biggest goals is to help improve communication between you and your care team, and with the OWise breast cancer app, there are a number of tools to help with this.
Using the Questions List feature, you can write down your urological and sexual health related questions so that you know exactly what you will ask before you arrive at the consultation. You can also make notes, store photos and audio-record your appointments so that later on you can check if you missed something important.
You can also check out our Glossary within the app for any terminology you want to brush up on.
Useful Links
Jo Divine Sex and Breast Cancer blog
Ticking Off Breast Cancer – Sex and Breast Cancer Q&A
Bladder control: Lifestyle strategies ease problems
References
- Ganz, Patricia A., et al. “Life after breast cancer: understanding women’s health-related quality of life and sexual functioning.” Journal of Clinical Oncology 16.2 (1998): 501-514.
- Trinkaus, Mateya, et al. “Should urogenital atrophy in breast cancer survivors be treated with topical estrogens?.” The oncologist 13.3 (2008): 222-231.
- Kelley, Charlotte. “Estrogen and its effect on vaginal atrophy in post-menopausal women.” Urol Nurs 27.1 (2007): 40-45.
- Nappi, Rossella E., et al. “Addressing vulvovaginal atrophy (VVA)/genitourinary syndrome of menopause (GSM) for healthy aging in women.” Frontiers in endocrinology 10 (2019): 561.
- Baumgart, Juliane, et al. “Urogenital disorders in women with adjuvant endocrine therapy after early breast cancer.” American journal of obstetrics and gynecology 204.1 (2011): 26-e1.
- Barlow, David H., et al. “Urogenital ageing and its effect on sexual health in older British women.” BJOG: An International Journal of Obstetrics & Gynaecology 104.1 (1997): 87-91.
- Cella, David, et al. “Quality of life of postmenopausal women in the ATAC (“Arimidex”, tamoxifen, alone or in combination) trial after completion of 5 years’ adjuvant treatment for early breast cancer.” Breast cancer research and treatment 100.3 (2006): 273-284.
- Minton, Susan E., and Pamela N. Munster. “Chemotherapy-induced amenorrhea and fertility in women undergoing adjuvant treatment for breast cancer.” Cancer Control 9.6 (2002): 466-472.
- Mourits, M. J., et al. “Tamoxifen effects on subjective and psychosexual well-being, in a randomised breast cancer study comparing high-dose and standard-dose chemotherapy.” British journal of cancer 86.10 (2002): 1546-1550.
- Mac Bride, Maire B., Deborah J. Rhodes, and Lynne T. Shuster. “Vulvovaginal atrophy.” Mayo Clinic Proceedings. Vol. 85. No. 1. Elsevier, 2010.
- Gupta, Pratima, et al. “The effect of transdermal and vaginal estrogen therapy on markers of postmenopausal estrogen status.” Menopause 15.1 (2008): 94-97.
- Loprinzi, Charles L., et al. “A Phase III randomized, double blind, placebo-controlled study of pilocarpine for vaginal dryness: NCCTG study N04CA.” The journal of supportive oncology 9.3 (2011): 105.
- Donovan, Kristine A., et al. “Urinary symptoms in breast cancer: a systematic review.” Cancer 118.3 (2012): 582-593.
- Krause, Megan, et al. “Local effects of vaginally administered estrogen therapy: a review.” Journal of pelvic medicine & surgery 15.3 (2009): 105.
- “Doxorubicin and Ifosfamide.” Macmillan Cancer Support, 1 Dec. 2020, www.macmillan.org.uk/cancer-information-and-support/treatments-and-drugs/doxorubicin-and-ifosfamide#:~:text=better for you.-,Bladder irritation,feel the need to go.
- “Bladder Problems – Canadian Cancer Society.” Www.cancer.ca, www.cancer.ca/en/cancer-information/diagnosis-and-treatment/managing-side-effects/bladder-problems/?region=on#:~:text=cause bladder problems.-,Chemotherapy,and lead to permanent damage.
- Karamanidis, D1, et al. “Cigarette smoking and the degree of maturation of the vaginal squamous epithelium in postmenopausal women.” Clinical and experimental obstetrics & gynecology 28.4 (2001): 274-276.
- Tähtinen, Riikka M., et al. “Smoking and bladder symptoms in women.” Obstetrics & Gynecology 118.3 (2011): 643-648.
- Chatsiproios, Dimitrios, et al. “Topical treatment of vaginal dryness with a non-hormonal cream in women undergoing breast cancer treatment-An open prospective multicenter study.” PloS one 14.1 (2019): e0210967.
- Keshavarzi, Zahra, et al. “The effect of vitamin D and E vaginal suppositories on tamoxifen-induced vaginal atrophy in women with breast cancer.” Supportive Care in Cancer 27.4 (2019): 1325-1334.
- Naumova, Iuliia, and Camil Castelo-Branco. “Current treatment options for postmenopausal vaginal atrophy.” International journal of women’s health 10 (2018): 387.
- https://www.fammed.wisc.edu/files/webfm-uploads/documents/research/wren/vva-breast-cancer-sheet.pdf
- Krishnamurthy, Jairam, and Pavan Kumar Tandra. “Genitourinary Syndrome of Menopause in Breast Cancer Survivors: A Common Complication With Effective Treatment Strategies.” Journal of oncology practice 15.7 (2019): 373-374.
- Cai, Bin, et al. “No increase in incidence or risk of recurrence of breast cancer in ospemifene-treated patients with vulvovaginal atrophy (VVA).” Maturitas 142 (2020): 38-44.
- “The Use of Vaginal Estrogen in Women With a History of Estrogen-Dependent Breast Cancer.” Revised from the May 2015 Version of Raising Awareness: Starting the Conversation by Ellen Barnard, MSSW, Anne Ford, MD, and Paul Smith, MD. , Mar. 2016, www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-opinion/articles/2016/03/the-use-of-vaginal-estrogen-in-women-with-a-history-of-estrogen-dependent-breast-cancer.pdf
- Ponzone, Riccardo, et al. “Vaginal oestrogen therapy after breast cancer: is it safe?.” European Journal of Cancer 41.17 (2005): 2673-2681.
- Knight, Charity, Vera Logan, and Deborah Fenlon. “A systematic review of laser therapy for vulvovaginal atrophy/genitourinary syndrome of menopause in breast cancer survivors.” ecancermedicalscience 13 (2019).
- Arroyo, César. “Fractional CO2 laser treatment for vulvovaginal atrophy symptoms and vaginal rejuvenation in perimenopausal women.” International journal of women’s health 9 (2017): 591.
- Cavkaytar, S., et al. “Effect of home-based Kegel exercises on quality of life in women with stress and mixed urinary incontinence.” Journal of Obstetrics and Gynaecology 35.4 (2015): 407-410.
- Park, Seong-Hi, and Chang-Bum Kang. “Effect of Kegel exercises on the management of female stress urinary incontinence: a systematic review of randomized controlled trials.” Advances in Nursing 2014 (2014).
- “Bladder Training Techniques.” WebMD, WebMD, www.webmd.com/urinary-incontinence-oab/bladder-training-techniques.
