Women reach menopause and fertility comes to an end, when they have no quality eggs (oocytes) left in the ovaries to ovulate, and have an effective period1. This leads to the ovaries producing less of the sex hormones estrogen, progesterone, and testosterone. Premature or early menopause can happen spontaneously or can be brought on by certain breast cancer treatments. If the menopause takes place before the age of 45 it is considered early menopause, if it happens before the age of 40 it is considered premature menopause2.
“Every woman will face the menopause and yet for so long it was almost a taboo conversation. By opening up honest conversations around it we can support one another through” – Carly Moosah, Breast Cancer Survivor
What are the sex hormones?
Estrogen, progesterone, and testosterone are sex hormones that are mainly made in the ovaries in women3. Sex hormones can also be made in the aromatase pathway. This is where androgens created in the adrenal glands are converted to estrogen. This happens all over the body, including in the liver, muscle but most significantly in the fat under the skin.
The sex hormones affect many processes in the body such as growth, puberty, periods, reproduction and menopause3. The level of sex hormones in the body changes naturally over time, but the right levels and balance of these hormones is key for the normal functioning of the body.
Breast cancer and menopause
Breast cancer is the most common cancer diagnosed in the US. Advances in breast cancer diagnosis and treatment have substantially improved survival rates of the disease, however, some medical interventions can trigger premature or early menopause in patients. Most women who receive a diagnosis are aged 50 or older. However, every year in the US, approximately 11,000 women under the age of 45 are diagnosed with breast cancer4. Menopause that is brought on early by breast cancer treatment can be either temporary or permanent. Permanence is more likely the closer in age you are to natural menopause and is also dependent on the treatment you are receiving5.
Breast cancer treatment and menopause
In cancer, there are several types of treatment that can cause early menopause, this is referred to as induced menopause. Treatments such as chemotherapy and hormone therapy, and surgical procedures such as removal of the ovaries (bilateral oophorectomy) can trigger early menopause. These are referred to as:
- Medical menopause e.g. chemotherapy, hormone therapy
- Surgical menopause e.g. bilateral oophorectomy
Induced menopause stops the ovaries from working and causes sex hormone levels to fall more suddenly than in natural menopause.
What is medical menopause?
Medical menopause can be temporary or permanent and can be brought on by treatments such as:
- Chemotherapy: Can destroy fast-dividing cells in the ovaries causing temporary or permanent damage
- Ovarian suppression: Drugs that stop estrogen being made in the ovaries such as goserelin (Zoladex®) and leuprorelin (Prostap®, Lutrate®)
- Tamoxifen and aromatase inhibitors: Do not induce menopause but can cause menopausal symptoms
Some women lose their periods are soon as they start chemotherapy, whereas others continue to have their periods during treatment. Usually, if a patient’s menstrual cycle is going to return this happens within 2 years of finishing treatment6. However, approximately, 10% of patients’ periods can return 3-5 years after the last cycle of chemotherapy7.
Ovarian suppression treatment prevents the ovaries from working for a limited period of time. They block the brain from telling the ovaries how to work, leading to a decrease of sex hormones in the body. Aromatase inhibitors have demonstrated significant benefits in preventing cancer recurrence and improving survival in post-menopausal women when compared to tamoxifen8. Aromatase inhibitors alone cannot be prescribed to pre-menopausal women as they cannot block the production of sex hormones in the ovaries. However, aromatase inhibitors can be prescribed to pre-menopausal women when combined with ovarian suppression. Ovarian suppressors can also be prescribed alongside tamoxifen or chemotherapy9.
Tamoxifen and aromatase inhibitors alone do not directly induce menopause. However, they can cause menopausal symptoms. Click to learn more about these side effects, including hot flushes, joint pain, sex-related, urogenital and tamoxifen-related side effects.
It is important to note that periods can return but this may not mean that the ovulation cycle is back to normal and the absence of a period does not necessarily indicate infertility. To learn more about fertility, check out the blog ‘Fertility and breast cancer‘.
What is surgical menopause?
Surgical menopause occurs when the ovaries are removed during a bilateral oophorectomy, the result is always permanent menopause. The sudden loss of ovarian function causes an immediate drop in hormone levels, meaning pre-menopausal patients can experience intense menopausal symptoms, particularly in women who were pre-menopausal.
How is menopause diagnosed?
The removal of the ovaries is certain to cause menopause. On the other hand, it is not guaranteed that drugs will trigger the menopause. In these cases, a diagnosis may be given. Typically, a diagnosis is given based on the symptoms associated with menopause, hormone levels and patient history6. Common and key symptoms include hot flushes, vaginal dryness and irregular or loss of menstrual periods. If you experience any of these symptoms, you may be diagnosed with menopause.
Menopause can also be diagnosed by blood test, which is common in those under the age of 4010. Blood tests measure hormone levels, which correlate to the onset of menopause. The blood test measures a sex hormone called Follicle Stimulating Hormone (FSH)11. If menopause is happening, there will be a high level of FSH compared to pre-menopausal women. However, this test is only accurate in women not on hormonal birth control, as this interferes with your FSH levels.
Menopause symptoms and management
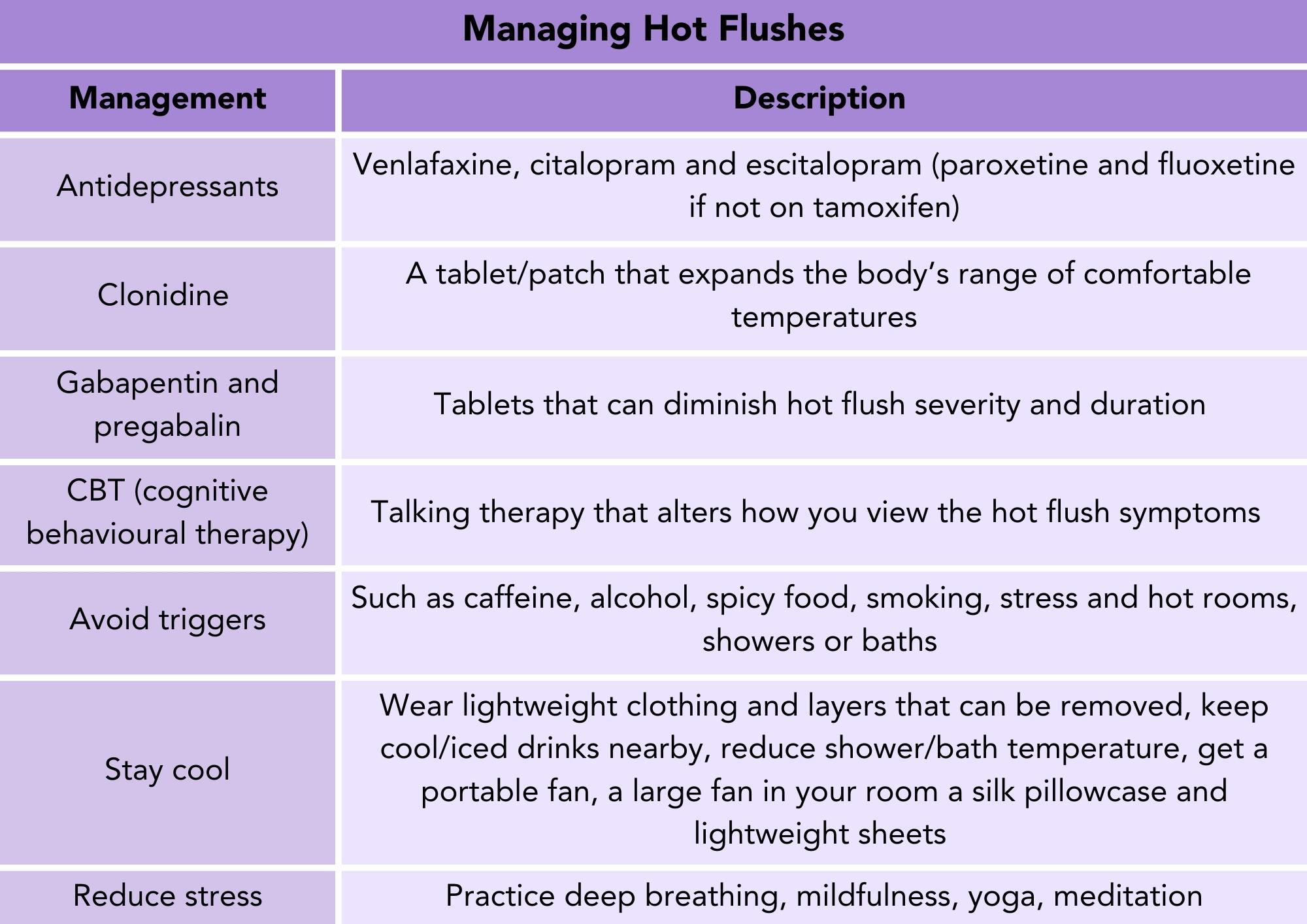
Hot flushes
Hot flushes are described as a sudden sensation of intense, internal heat in the chest, face and head, accompanied by potential flushing, chills and sweating. They are thought to occur as an inflated exaggerated bodily response to normal changes in heat12,13. Research indicates that hot flushes resulting from hormone therapy, such as tamoxifen or ovarian suppression are typically more intense than those experienced during natural menopause, and symptoms following chemotherapy or ovarian suppression tend to be even more severe than those associated with tamoxifen6.
There are several medical interventions and lifestyle changes available that can help to manage hot flushes. A few antidepressant drugs have been shown to reduce severity and frequency of hot flushes14. Although, paroxetine and fluoxetine must be avoided if you are taking tamoxifen. For more information on this check out our article ‘Tamoxifen: what you should and shouldn’t avoid’.
In addition, a drug that is usually prescribed for high blood pressure, Clonidine, and drugs prescribed to treat epilepsy gabapentin and pregabalin, have been shown to effectively manage hot flushes. Another medical intervention available to manage hot flushes is cognitive behavioral therapy (CBT). This is a type of talk therapy that has proven effective in managing menopausal symptoms. It focuses on altering how you view the symptoms rather than their frequency15.
There are certain lifestyle changes that can be incorporated that may help to ease hot flushes. For example, avoiding things that trigger your hot flushes, taking steps to stay as cool as possible, and reducing stress in your life.
Table 1. Treatments and strategies to manage hot flushes
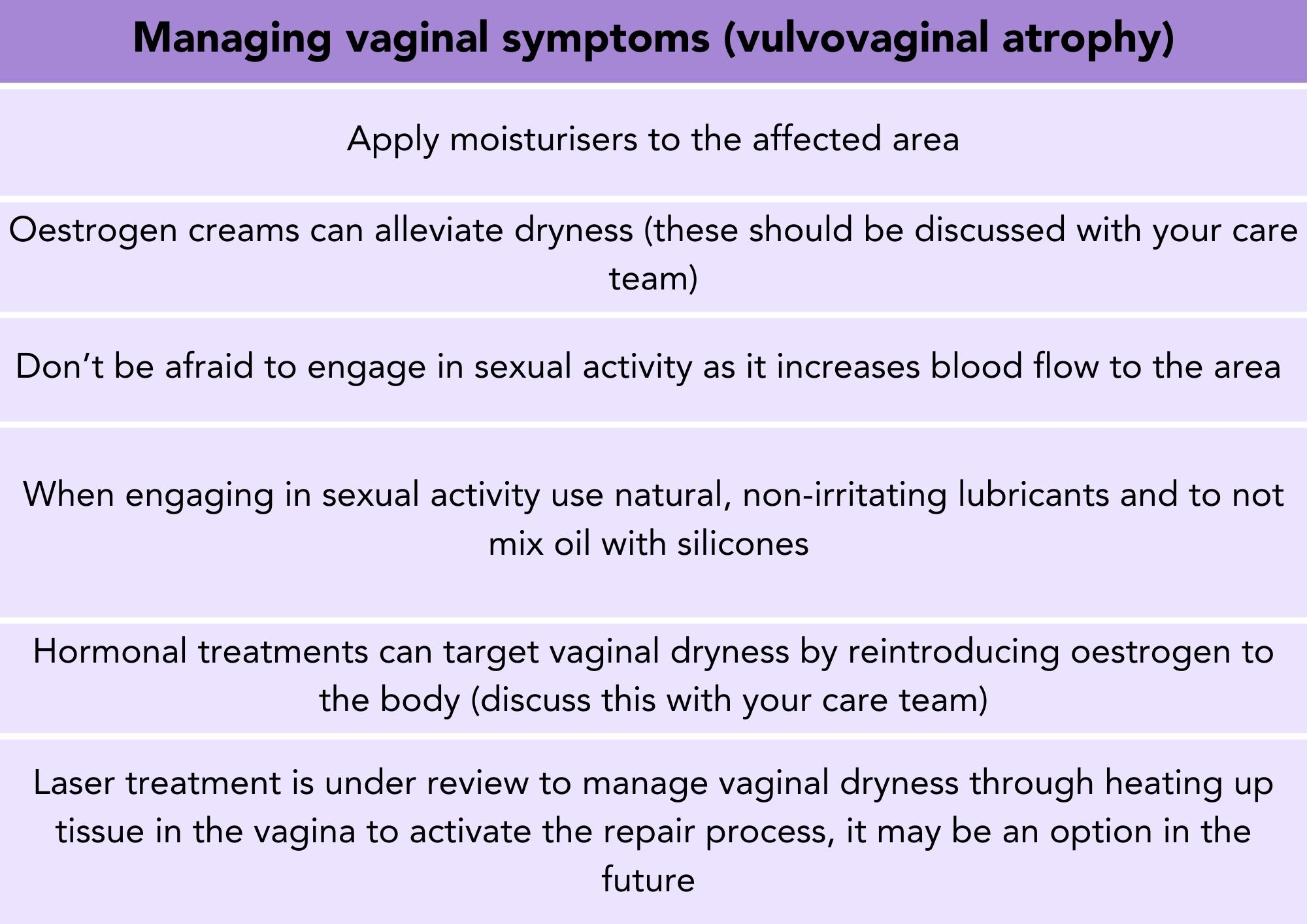
Sexual side effects
Hormone therapies and ovarian suppression can cause vulvovaginal atrophy, which is responsible for causing symptoms such as vaginal dryness, burning, discharge, itchiness, irritation, and bleeding16. These are brought on by the reduction in estrogen in the body17. Approximately 50-75% of people with breast cancer can experience at least one symptom related to their genital and urinary areas, including problems with the vulva, vagina and urinary tract18,19. This can result in pain during intercourse, leading to a loss of sexual desire and reduced libido. Other symptoms caused by breast cancer treatment can also impact sexual function indirectly, such as hair loss, fatigue and body image.
Table 2. Strategies to manage vaginal symptoms
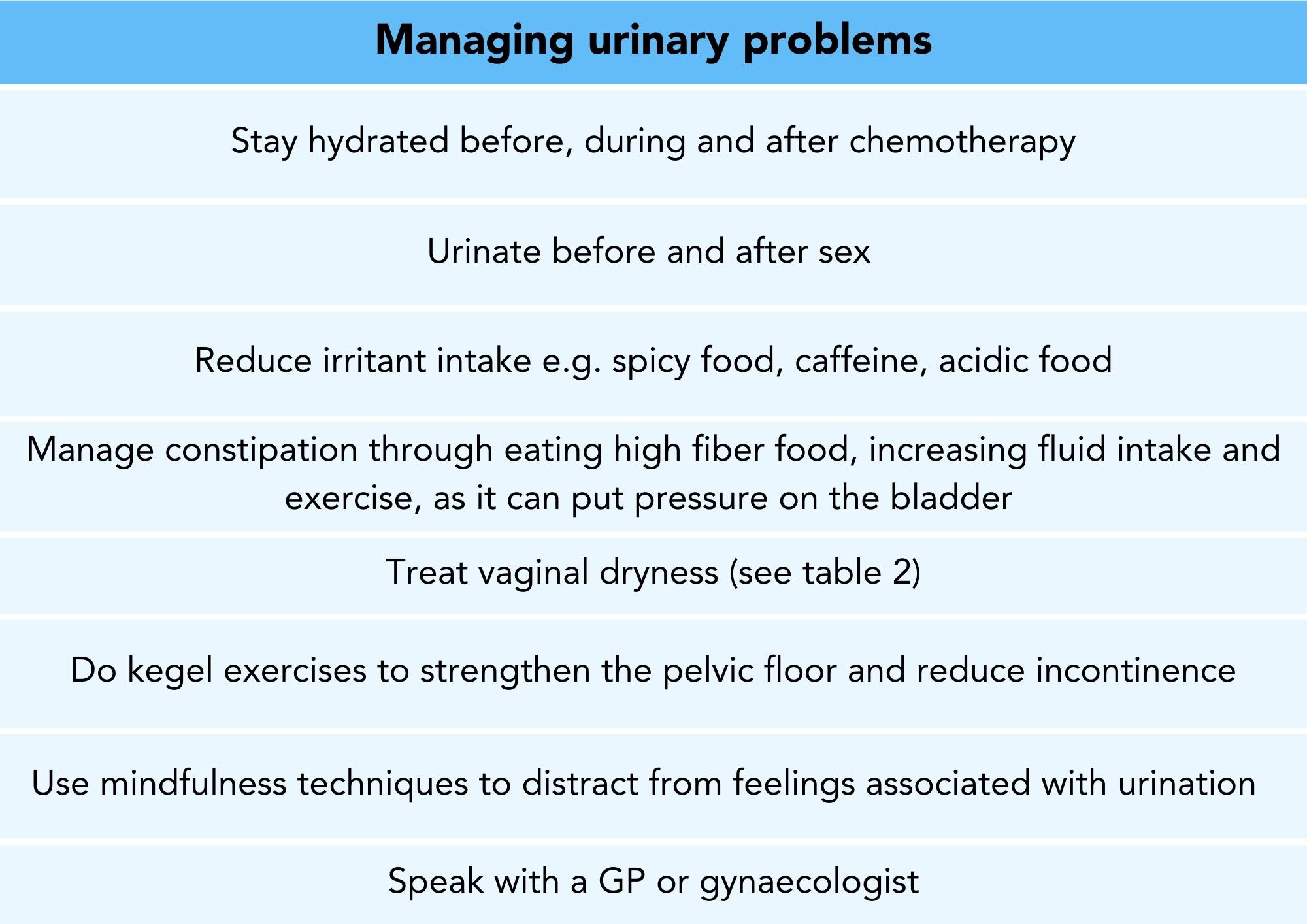
Table 3. Strategies to manage urinary problems
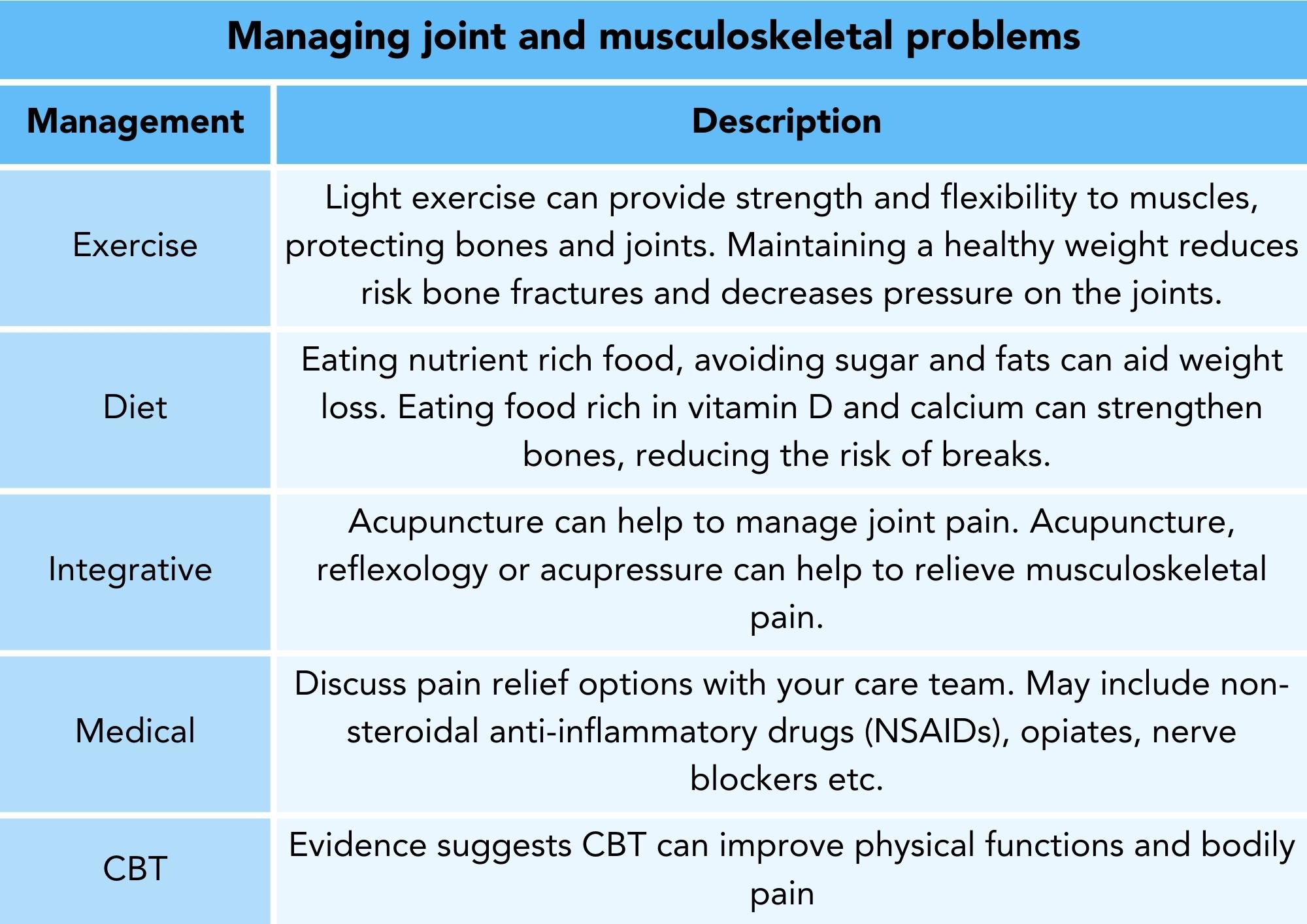
Joint and musculoskeletal problems
Aromatase inhibitors used in breast cancer treatment commonly cause joint and musculoskeletal side effects. This is due to a reduction in oestrogen in the body, which increases the risk of osteoporosis (weakened bones) due to accelerated bone loss20. Additionally, it can cause joint stiffness (arthralgia), most commonly in the fingers, wrists, knees, and ankles21. There is a similar estrogen reduction during menopause which is why there is an increased risk of bone thinning associated22. Instead of causing pain in the joints directly, estrogen plays a role in inflammation. This affects the nearby nerves and causes pain sensations23. Research suggests there is an increased risk of arthralgia if previous treatment with taxane-based chemotherapy has been received6.
Exercise has been demonstrated to be beneficial in improving joint and musculoskeletal pain and can permanently improve joint point and quality of life24. Workouts such as light weight bearing movements, frequent walks, yoga and pilates are great options for effective and gentle exercise. Maintaining a healthy and balanced diet can aid weight loss which can relieve pressure on bones and joints. Additionally, eating vitamin D and calcium rich foods can strengthen bones and reduce the risk of breaks.
There are multiple pain relief medications available that should be discussed with your care team. CBT has also demonstrated benefits in improving physical functions and bodily pain in patients with joint pain26. Alternatively, there is evidence to suggest some integrative approaches may be effective at managing, including acupuncture for aromatase inhibitor induced joint pain and acupuncture, reflexology or acupressure for musculoskeletal pain25.
Table 4. Strategies to manage joint and musculoskeletal problems
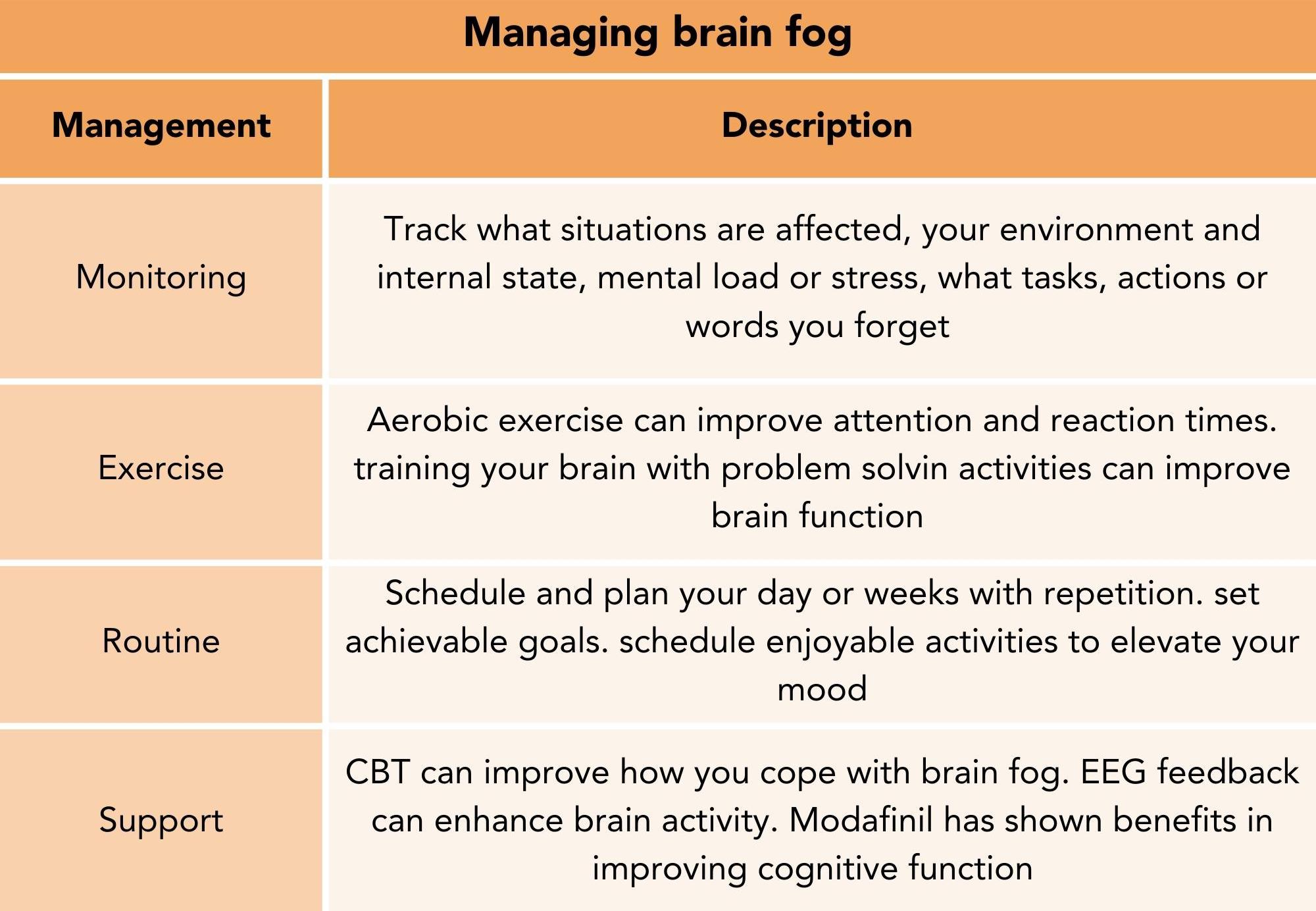
Cognitive dysfunction (Brain fog)
Cancer related cognitive dysfunction (CRCD), also known as chemobrain or brain fog, includes issues with attention, learning, memory, processing speed and psychological wellbeing. Reports show that up to 75% of breast cancer patients on treatment and 35% of breast cancer survivors experience brain fog27,28. Although brain fog is commonly associated with chemotherapy, other treatments can also cause problems with brain function27. Brain fog can cause issues in many aspects of daily life, such as remembering things to do in the future, things that happened in the past, and problem-solving activities.
“I welcome the menopause and the woman I am with it. I accept the halts in conversation as I try and grasp at what it is I’m trying to say and it teaches me the lessons in letting go. I embrace the body changes that have seen my weight go up, but my love for this vessel go up with it too” – Carly Moosah, Breast Cancer Survivor
Brain fog can be managed through effectively monitoring symptoms. This can enable you to learn what situations are high risk for you and recognize patterns in issues surrounding your brain function. There is evidence to suggest that exercise can enhance many brain functions. Additionally, cognitive training, such as sudoku and problem-solving activities, enhance brain plasticity, which is how effectively the brain can grow, adapt, and learn. Establishing a routine can be beneficial when trying to deal with brain fog. Scheduling and planning your day, or weeks with repetition, setting achievable goals, and scheduling in fun and enjoyable activities to elevate your mood can all help you deal with and manage brain fog.
As well as this, there are medical interventions available to help to manage brain fog. CBT can be useful to improve cognitive function deterioration after cancer treatment. EEG biofeedback is a method that monitors and enhances brain activity using visual or auditory cues, and is showing promising results in improving cognitive outcomes, fatigue, depression, anxiety, and sleep among breast cancer survivors29. Modafinil, a stimulant, has shown potential benefits in memory, attention, and overall cognitive function for breast cancer patients30.
Table 5. Strategies to manage brain fog
Did you know you can keep track of your menopausal symptoms using the OWise app? Choose from 30+ side effects and track how you are feeling using https://owi.se/dlsliders on the app. Visualise how your trends change over time through the graphs and share this data directly with your care team.
Heart disease and menopause
Both natural and induced menopause are associated with a higher risk of cardiovascular disease, this refers to any problems that affect the heart and blood vessels. Researchers are not yet sure exactly what the role of estrogen is in cardiovascular disease, but it is thought it could be involved in protecting women’s heart and blood vessels when they are younger31. The risk of heart disease can be reduced by not smoking, regular exercise, stress reduction, healthier diet, and healthy body weight maintenance.
Hormone replacement therapy (HRT) and breast cancer
Hormone replacement therapy (HRT) is treatment that replaces hormones that are at a low level during menopause and can relieve menopausal symptoms32. However, at present HRT is not recommended in women who previously or currently have HR+ breast cancer33.
We hope that you now have a good understanding of early menopause, how it can be induced by breast cancer treatment, symptoms associated with it and ways of managing them. At OWise, we want to make sure you are kept informed so make sure to follow our Instagram and Facebook for any updates. Any questions? Get in touch!
References
- Buckler H. The menopause transition: endocrine changes and clinical symptoms. British Menopause Society Journal. 2005;11(2):61–65. doi:https://doi.org/10.1258/136218005775544525
- Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA. Premature menopause or early menopause: Long-term health consequences. Maturitas. 2010;65(2):161–166. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2815011/. doi:https://doi.org/10.1016/j.maturitas.2009.08.003
- Aliouche H. An Overview Of Sex Hormones. News-Medical.net. 2022. https://www.news-medical.net/health/An-Overview-Of-Sex-Hormones.aspx
- Breast Cancer Now. Younger women with breast cancer. https://breastcancernow.org/sites/default/files/publications/pdf/bcc66_younger_women_with_breast_cancer_web.pdf.
- Breast Cancer. How Menopause Can Happen With Breast Cancer Treatments. www.breastcancer.org. 2022. https://www.breastcancer.org/treatment-side-effects/menopause/types/cancer-treatment-caused
- Marsden J, Marsh M, Rigg A. British Menopause Society consensus statement on the management of estrogen deficiency symptoms, arthralgia and menopause diagnosis in women treated for early breast cancer. Post Reproductive Health. 2019;25(1):21–32. doi:https://doi.org/10.1177/2053369118824920
- Sukumvanich P, Case LD, Van Zee K, Singletary SE, Paskett ED, Petrek JA, Naftalis E, Naughton MJ. Incidence and time course of bleeding after long-term amenorrhea after breast cancer treatment. Cancer. 2010;116(13):3102–3111. doi:https://doi.org/10.1002/cncr.25106
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. The Lancet. 2015;386(10001):1341–1352. doi:https://doi.org/10.1016/s0140-6736(15)61074-1
- Breast Cancer Now. Ovarian suppression and breast cancer. 2022. https://breastcancernow.org/about-breast-cancer/treatment/hormone-endocrine-therapy/ovarian-suppression-and-breast-cancer/#7-how-long-do-i-need-ovarian-suppression-for
- NHS Inform. Information around the symptoms of menopause. www.nhsinform.scot. 2023. https://www.nhsinform.scot/healthy-living/womens-health/later-years-around-50-years-and-over/menopause-and-post-menopause-health/signs-and-symptoms-of-menopause#:~:text=Your%20GP%20can%20usually%20confirm
- Menopause: diagnosis and management. www.nice.org.uk. 2015. https://www.nice.org.uk/guidance/ng23/ifp/chapter/diagnosing-menopause#:~:text=The%20blood%20test%20measures%20a
- Freedman RR. Physiology of hot flashes. American Journal of Human Biology. 2001;13(4):453–464. doi:https://doi.org/10.1002/ajhb.1077
- Rossmanith WG, Ruebberdt W. What causes hot flushes? The neuroendocrine origin of vasomotor symptoms in the menopause. Gynecological Endocrinology. 2009;25(5):303–314. doi:https://doi.org/10.1080/09513590802632514
- Carroll DG, Kelley KW. Use of Antidepressants for Management of Hot Flashes. Pharmacotherapy. 2009;29(11):1357–1374. doi:https://doi.org/10.1592/phco.29.11.1357
- Women’s Health Concern. Cognitive Behaviour Therapy (CBT) for Menopausal Symptoms WOMEN’S HEALTH CONCERN FACT SHEET Information for women. 2022. https://www.womens-health-concern.org/wp-content/uploads/2023/02/02-WHC-FACTSHEET-CBT-WOMEN-FEB-2023-A.pdf
- Nappi RE, Martini E, Cucinella L, Martella S, Tiranini L, Inzoli A, Brambilla E, Bosoni D, Cassani C, Gardella B. Addressing Vulvovaginal Atrophy (VVA)/Genitourinary Syndrome of Menopause (GSM) for Healthy Aging in Women. Frontiers in Endocrinology. 2019;10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6712495/. doi:https://doi.org/10.3389/fendo.2019.00561
- Baumgart J, Nilsson K, Anneli Stavréus-Evers, Kask K, Villman K, Lindman H, Theodora Kunovac Kallak, Sundström‐Poromaa I. Urogenital disorders in women with adjuvant endocrine therapy after early breast cancer. American Journal of Obstetrics and Gynecology. 2011;204(1):26.e1–26.e7. doi:https://doi.org/10.1016/j.ajog.2010.08.035
- Ganz PA, Rowland JH, Desmond K, Meyerowitz BE, Wyatt GE. Life after breast cancer: understanding women’s health-related quality of life and sexual functioning. Journal of Clinical Oncology. 1998 [accessed 2021 Mar 18];16(2):501–514. doi:https://doi.org/10.1200/jco.1998.16.2.501
- Trinkaus M, Chin S, Wolfman W, Simmons C, Clemons M. Should Urogenital Atrophy in Breast Cancer Survivors Be Treated with Topical Estrogens? The Oncologist. 2008;13(3):222–231. doi:https://doi.org/10.1634/theoncologist.2007-0234
- Weitzmann MN. Estrogen deficiency and bone loss: an inflammatory tale. Journal of Clinical Investigation. 2006;116(5):1186–1194. doi:https://doi.org/10.1172/jci28550
- Younus J, Kligman L. Management of aromatase inhibitor-induced arthralgia. Current Oncology. 2010;17(1). doi:https://doi.org/10.3747/co.v17i1.474
- Endocrine Society. Menopause and Bone Loss. www.endocrine.org. 2022. https://www.endocrine.org/patient-engagement/endocrine-library/menopause-and-bone-loss#:~:text=As%20hormones%20change%20to%20accommodate
- Felson DT, Cummings SR. Aromatase inhibitors and the syndrome of arthralgias with estrogen deprivation. Arthritis & Rheumatism. 2005;52(9):2594–2598. doi:https://doi.org/10.1002/art.21364
- Lu G, Zheng J, Zhang L. The effect of exercise on aromatase inhibitor-induced musculoskeletal symptoms in breast cancer survivors :a systematic review and meta-analysis. Supportive Care in Cancer. 2019;28(4). doi:https://doi.org/10.1007/s00520-019-05186-1
- Mao JJ, Ismaila N, Bao T, Barton D, Ben-Arye E, Garland EL, Greenlee H, Leblanc T, Lee RT, Lopez AM, et al. Integrative Medicine for Pain Management in Oncology: Society for Integrative Oncology–ASCO Guideline. Journal of Clinical Oncology. 2022;40(34). doi:https://doi.org/10.1200/jco.22.01357
- Mann E, Smith MJ, Hellier J, Balabanovic JA, Hamed H, Grunfeld EA, Hunter MS. Cognitive behavioural treatment for women who have menopausal symptoms after breast cancer treatment (MENOS 1): a randomised controlled trial. The Lancet Oncology. 2012;13(3):309–318. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3314999/. doi:https://doi.org/10.1016/s1470-2045(11)70364-3
- Jean-Pierre P. Management of Cancer-related Cognitive Dysfunction—Conceptualization Challenges and Implications for Clinical Research and Practice. Oncology & Hematology Review (US). 2010;6(1):9. doi:https://doi.org/10.17925/ohr.2010.06.0.9
- Janelsins MC, Kesler SR, Ahles TA, Morrow GR. Prevalence, mechanisms, and management of cancer-related cognitive impairment. International Review of Psychiatry. 2014;26(1):102–113. doi:https://doi.org/10.3109/09540261.2013.864260
- Luctkar-Flude M, Tyerman J, Groll D. Exploring the Use of Neurofeedback by Cancer Survivors: Results of Interviews with Neurofeedback Providers and Clients. Asia-Pacific Journal of Oncology Nursing. 2019;6(1):35. doi:https://doi.org/10.4103/apjon.apjon_34_18
- Kohli S, Fisher SG, Tra Y, Wesnes K, Morrow GR. The cognitive effects of modafinil in breast cancer survivors: A randomized clinical trial. Journal of Clinical Oncology. 2007;25(18_suppl):9004–9004. doi:https://doi.org/10.1200/jco.2007.25.18_suppl.9004
- Breast Cancer. Cardiovascular Health After Menopause. www.breastcancer.org. 2022. https://www.breastcancer.org/treatment-side-effects/menopause/long-term-health/cardiovascular-health
- Hormone replacement therapy (HRT). nhs.uk. 2023 Jul 21. https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/
- Hormone replacement therapy (HRT). NICE. 2022. https://cks.nice.org.uk/topics/menopause/prescribing-information/hormone-replacement-therapy-hrt/#contraindications-cautions